All food is made up of complex mixtures of carbohydrates, proteins and fats. These need to be broken down by our digestive system via enzymes into much simpler single sugars, amino acids and fatty acids in order for us to absorb and use these to produce energy. When this process is not working well, we can suffer from nutritional deficiencies and malabsorption.
All food is made up of complex mixtures of carbohydrates, proteins and fats. These need to be broken down by our digestive system via enzymes into much simpler single sugars, amino acids and fatty acids in order for us to absorb and use these to produce energy. When this process is not working well, we can suffer from nutritional deficiencies and malabsorption.
Digestive enzymes break down our food
When your food is not digested properly, the environment for your microbiome and your beneficial bacteria can be altered1. Impaired digestion can lead to symptoms of ‘IBS’ such as irregular bowel movements, diarrhoea, constipation, flatulence and cramping2.
Some enzymes also breakdown inflammatory signals in the gut such as bacterial products like LPS and flagellin which would normally trigger an immune response. Reduced protection from these enzymes has been demonstrated in intestinal bowel diseases, contributing to chronic inflammation and damage to the gut barrier.3
Symptoms of poor digestion
- Nutritional deficiencies and related symptoms such as fatigue, poor hail and nail condition among many other signs
- Belching, reflux
- Bloating and discomfort
- Feeling of the food not moving on down or uncomfortable feelings of fullness even after eating relatively small meals
- ‘IBS’ symptoms such as cramps, spasms and irregular bowel movements
Digestion begins in the mouth
Food first encounters digestive enzymes in the mouth as the saliva we produce contains amylase to breakdown starch and lingual lipase to begin breaking down fats. Acid in our stomach will make headway then on proteins and fats from our meals. Food usually churns about in our stomach for about an hour before moving on into the duodenum and the small intestine.
Pancreatic enzymes
When food leaves our stomach, the pancreas is triggered to release important digestive enzymes. Pancreatic insufficiency can be transient, in the case of impaired activation by your gut, or reduced output which could be post-viral. Chronic pancreatic insufficiency can also occur in some conditions such as chronic pancreatitis, pancreatic cancer and cystic fibrosis.
The main pancreatic enzymes are:
- Lipase – breakdown of fats, working together with bile, which your liver produces
- Protease – breakdown of proteins
- Amylase – breakdown of starches into simple sugars for absorption
Replacement enzyme therapy may be prescribed by your doctor in the form of Creon which contains these three enzymes, but lacks any other enzyme support.
Brush border enzymes
Brush border enzymes are produced in the small intestine, the next step after pancreatic digestion. The brush border is the term for the bristle-like lining of the small intestine which is adapted to absorb nutrients effectively from our food. Along with pancreatic enzymes, that do some of the heavy lifting, there are a number of enzymes produced here at this interface. These can be secreted out into the gut space as a pre-absorptive measure – to break down the sugars, carbs and proteins which the cells lining the gut will then absorb. A good broad spectrum digestive enzyme should include some of these brush border enzymes.
We cannot currently test the production of these enzymes, only the pancreatic enzyme output in the form of elastase. This is a good marker of pancreatic output. We may also need to support the brush border enzymes though, even if the pancreatic output is good. Generally supporting the health of the gut lining and the environment in the gut can support this process and improve absorption of nutrients.
Digestive enzyme supplements
Based on your symptoms and tolerance of certain foods, your Nutritional Therapist may recommend trying a digestive enzyme supplement with a broad spectrum of enzymes. It is important to note that some digestive enzyme supplements can be very strong. Some can include HCl, which is the acid found in the stomach. These supplements can be very irritating or damaging if there is already inflammation in the stomach or the gut. If you have been diagnosed with oesophagitis, ulcers, gastritis or any other form of gut inflammation, it is important to get advice on these supplements. We would not recommend trying any digestive supplements without advice or supervision.
Testing digestive enzymes and pancreatic function
We use a comprehensive stool analysis which includes a measurement of pancreatic elastase. This test also includes markers of inflammation and much information on the health of the gut lining and the microbiome. All of these factors will be taken into account before recommending a safe supplement protocol. If the level or pancreatic elastase is very low, we may refer you to a consultant for follow up. Working on supporting the whole digestive process and health of the gut can improve pancreatic output and improve overall digestion and health.
Case example:
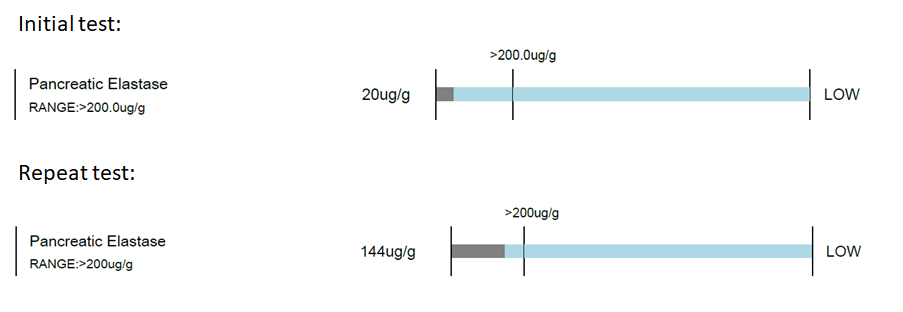
Female age 78 – loss of weight, fatigue, cramps, unable to tolerate normal portions in meals. Pancreatic elastase measured at 20ug/g (normal range above 200ug/g), no inflammation detected. This patient was supported with dietary advice and a comprehensive supplement protocol. Her GP reviewed the digestive enzyme support and was happy for her to proceed instead of prescribing the medicated version. After 12 months, a repeat pancreatic elastase showed her level had improved to 144ug/g. We are still working to support her digestive health but this was a significant improvement. Her fatigue and general wellness had improved significantly and she had gained weight indicating improved absorption from her diet.
Bilski, J., et al (2017). The Role of Intestinal Alkaline Phosphatase in Inflammatory Disorders of Gastrointestinal Tract. Mediators of inflammation, 2017, 9074601. https://doi.org/10.1155/2017/9074601